Schwannoma Tumor Spine

Schwannomas are rare benign tumors that arise from the Schwann cells, which are responsible for producing the myelin sheath that surrounds and protects the peripheral nerves. While these tumors can develop in various parts of the body, they often occur in the head, neck, and spinal regions. In this article, we delve into the specifics of Schwannoma tumors affecting the spine, shedding light on their characteristics, diagnosis, treatment options, and the latest advancements in managing this condition.
Understanding Schwannoma Tumors of the Spine
Schwannoma tumors, when present in the spine, are typically slow-growing and non-cancerous. They originate from the Schwann cells that wrap around the nerve fibers, providing insulation and facilitating efficient nerve signal transmission. These tumors can arise from any nerve in the spine, and their size can vary significantly, ranging from a few millimeters to several centimeters.
One unique aspect of spinal Schwannomas is their propensity to develop within the spinal nerve roots or the spinal cord itself. This makes them distinct from other spinal tumors, as they directly impact the nervous system. As the tumor grows, it can compress nearby structures, leading to a range of neurological symptoms that vary depending on the tumor's location and size.
Spinal Schwannomas are often categorized based on their location along the spine. They can be found in the cervical (neck), thoracic (upper back), or lumbar (lower back) regions, each presenting with different clinical manifestations and treatment considerations.
Common Symptoms of Spinal Schwannomas
The symptoms associated with spinal Schwannomas are primarily neurological in nature and can include:
- Pain and Discomfort: Patients often experience localized pain in the affected region of the spine. This pain may radiate to nearby areas, such as the arms or legs, depending on the tumor’s location.
- Sensory Changes: Schwannomas can cause numbness, tingling, or a reduced sensation in the areas supplied by the affected nerve.
- Motor Weakness: In some cases, the tumor’s growth can compress the spinal cord or nerve roots, leading to muscle weakness or even paralysis in severe instances.
- Balance and Coordination Issues: Larger tumors, especially those in the cervical spine, can affect balance and coordination, potentially causing gait disturbances or difficulty with fine motor skills.
- Bowel and Bladder Dysfunction: Tumors located in the lumbar region may impact the nerves controlling bowel and bladder function, leading to incontinence or other related issues.
It's important to note that the severity and specific symptoms can vary greatly from person to person, and early diagnosis is crucial for effective management.
Diagnosis and Detection of Spinal Schwannomas

Diagnosing spinal Schwannomas typically involves a combination of clinical evaluation, imaging techniques, and sometimes, nerve function tests.
Clinical Evaluation
Neurologists or spine specialists will conduct a thorough medical history review and perform a comprehensive neurological examination. They will assess the patient’s symptoms, including the duration and severity of pain, sensory changes, and any motor function deficits.
Imaging Techniques
Advanced imaging plays a crucial role in diagnosing spinal Schwannomas. Common imaging modalities include:
- Magnetic Resonance Imaging (MRI): MRI scans are highly sensitive in detecting spinal tumors. They provide detailed images of the spinal cord, nerve roots, and surrounding structures, helping to identify the tumor’s location, size, and any associated complications.
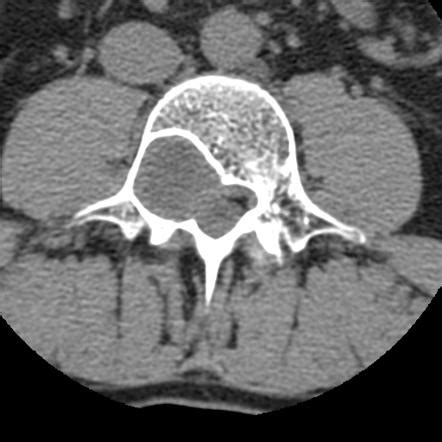
- Computed Tomography (CT) Scan: CT scans can be useful in certain cases, especially when assessing bone involvement or evaluating potential spinal instability caused by the tumor.
- Myelography: This technique involves injecting a contrast dye into the spinal canal, followed by an X-ray or CT scan. Myelography can help visualize the spinal cord and nerve roots, aiding in the diagnosis of spinal tumors.
Nerve Function Tests
Electromyography (EMG) and nerve conduction studies (NCS) may be performed to assess the function and integrity of the nerves affected by the tumor. These tests can help determine the extent of nerve damage and guide treatment decisions.
Treatment Options for Spinal Schwannomas
The management of spinal Schwannomas depends on various factors, including the tumor’s size, location, growth rate, and the patient’s overall health. The primary goal of treatment is to alleviate symptoms, prevent further neurological deterioration, and maintain the patient’s quality of life.
Surgical Intervention
Surgery is often the preferred treatment for spinal Schwannomas, especially when the tumor is causing significant symptoms or is growing rapidly. Surgical approaches can vary depending on the tumor’s location and the surgeon’s expertise.
For tumors located in the cervical or thoracic spine, surgeons may perform a procedure called anterior cervical discectomy and fusion (ACDF) or a cervical corpectomy. These techniques involve accessing the tumor from the front of the neck, removing the affected vertebrae and tumor, and stabilizing the spine with a fusion procedure. This approach helps preserve the spinal cord and nerve roots.
In cases where the tumor is located in the lumbar spine, surgeons may opt for a posterior lumbar decompression or a laminectomy. These procedures involve accessing the tumor from the back, removing the tumor, and potentially stabilizing the spine if necessary.
Minimally invasive surgical techniques are also gaining popularity, offering smaller incisions, reduced trauma, and faster recovery times. These approaches often involve the use of endoscopes or specialized instruments to access and remove the tumor.
Radiation Therapy
In certain situations, radiation therapy may be recommended as an adjunctive treatment or as a primary treatment option. Stereotactic radiosurgery, for instance, delivers precise radiation doses to the tumor, minimizing damage to surrounding healthy tissues. This approach is particularly useful for tumors that are difficult to access surgically or when surgery is not an option due to the patient’s health status.
Observation and Monitoring
For small, asymptomatic spinal Schwannomas, a conservative approach involving close observation and regular imaging may be chosen. This strategy is particularly applicable when the tumor is not causing any symptoms and is not growing rapidly. Patients will undergo periodic MRI scans to monitor the tumor’s behavior and ensure it remains stable.
Prognosis and Long-Term Management
The prognosis for patients with spinal Schwannomas is generally positive, especially when the tumor is detected and treated early. Surgical resection often leads to significant symptom relief and improved quality of life. However, as with any surgical procedure, there are potential risks and complications, including infection, bleeding, and nerve damage.
Post-operative care is crucial, and patients typically undergo rehabilitation to regain strength and mobility. Follow-up appointments with their healthcare team are essential to monitor for any potential tumor recurrence or new symptoms.
In cases where the tumor cannot be completely removed, ongoing surveillance and management are necessary. Regular imaging and clinical assessments help detect any changes in the tumor's behavior and allow for timely interventions.
Emerging Treatment Approaches
Advancements in medical technology and research are leading to innovative treatment options for spinal Schwannomas. These include:
- Targeted Drug Therapies: Researchers are exploring the use of targeted drugs that specifically act on the genetic abnormalities associated with Schwannoma tumors. These therapies aim to shrink the tumor and reduce its growth rate.
- Immunotherapy: Immunotherapy approaches are being investigated to harness the body’s immune system to fight against Schwannoma cells. Early clinical trials show promising results, offering a potential new avenue for treatment.
- Genetic Testing and Precision Medicine: Genetic testing can help identify specific mutations or biomarkers present in Schwannoma tumors. This information can guide the selection of targeted therapies, improving treatment outcomes.
Real-World Case Study: A Patient’s Journey

To illustrate the impact of spinal Schwannomas and the treatment journey, let’s consider the case of Mr. Johnson, a 48-year-old patient who presented with neck pain and numbness in his left arm.
Mr. Johnson's symptoms had been gradually worsening over several months, prompting him to seek medical attention. After a thorough clinical evaluation and an MRI scan, a spinal Schwannoma was diagnosed in the cervical region of his spine. The tumor was causing compression of the left C6 nerve root, leading to his neurological symptoms.
Given the tumor's size and location, the medical team recommended surgical intervention. Mr. Johnson underwent an anterior cervical discectomy and fusion procedure, successfully removing the tumor and decompressing the affected nerve root. The surgery was followed by a period of rehabilitation, during which he regained strength and mobility in his arm.
Post-operatively, Mr. Johnson experienced significant relief from his symptoms, and follow-up MRI scans showed no signs of tumor recurrence. He continues to be monitored regularly by his healthcare team, ensuring his long-term well-being.
Conclusion
Spinal Schwannomas, while rare, can have a significant impact on an individual’s life. Early diagnosis and appropriate treatment planning are crucial for managing these tumors effectively. With advancements in surgical techniques, radiation therapy, and emerging targeted therapies, patients with spinal Schwannomas can look forward to improved outcomes and a better quality of life.
Can spinal Schwannomas be cancerous?
+Spinal Schwannomas are typically benign and non-cancerous. However, in rare cases, they can undergo malignant transformation, becoming malignant peripheral nerve sheath tumors. Regular follow-up and monitoring are crucial to detect any changes in the tumor’s behavior.
Are there any risk factors associated with spinal Schwannomas?
+While the exact cause of spinal Schwannomas is not fully understood, certain genetic conditions, such as Neurofibromatosis type 2 (NF2), can increase the risk. Additionally, exposure to certain chemicals or radiation may play a role, but more research is needed to establish these connections.
How common are spinal Schwannomas, and who is at risk?
+Spinal Schwannomas are relatively rare, with an incidence rate of about 1 in 100,000 people. They can occur at any age, but they are more commonly diagnosed in adults, with a slightly higher prevalence in women. Individuals with certain genetic conditions, such as NF2, are at a higher risk.



